The COVID-19 pandemic has had a profound impact on the American healthcare system, causing disruptions and driving rapid adaptations to care delivery. Whether these changes will be temporary or permanent remains to be seen. In the meantime, repercussions are being realized – from the patient experience to ultimate health outcomes – by all healthcare consumers, including injured workers.
The degree to which patients are affected by the transforming healthcare landscape can vary, depending on factors such as geography, disease/condition, etc. But some changes are likely to impact most, if not all, workers’ compensation patients.

Receiving care in a timely manner is essential for injured workers to recover fully and return to work as quickly as possible. Even before COVID-19, physician shortages and the administrative requirements of the highly regulated workers’ compensation healthcare environment were contributing to longer wait times for injured workers in some areas, and the risk of delayed care has been exacerbated by pandemic-induced changes, including:

Unfortunately, the patients who most need to see their physicians – those with chronic conditions – are also the most likely to delay care. These patients are particularly wary of medical environments because their conditions make them susceptible to severe illness and death from COVID-19.
In fact, death rates are 12 times higher for patients with chronic conditions, regardless of age.3 However, it is also crucial that these patients receive consistent care to manage these conditions, which can lead to a host of serious complications unrelated to COVID-19.
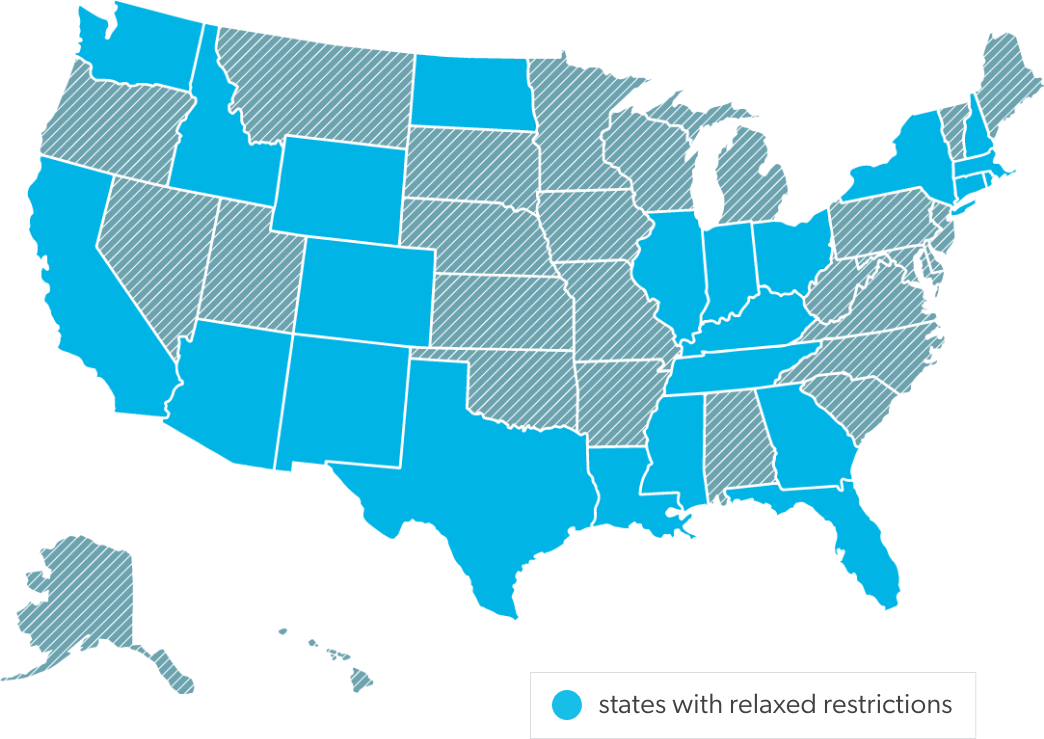
One way to mitigate care access issues is by using telemedicine, which makes it possible for more patients to avoid unnecessary exposure by consulting with physicians virtually. Since the pandemic began, 5% of the U.S. population, or 16.5 million people, has used telehealth services.5 This includes workers’ comp patients in at least 24 states7 where legislators have rushed to pass laws removing or relaxing restrictions on telehealth visits.
Telemedicine has also been helpful in allowing patients to continue physical and behavioral therapies. One service provider reported a 650% increase in telerehab referrals,8 and a large insurer reported telemedicine use for behavioral health has increased by 56 times, as compared to pre-COVID-19 levels.9 For workers’ comp patients, such remote services can be indispensable to keeping a full and timely recovery on course. At Healthesystems, we saw a nearly 20-fold increase in telerehab appointments from March to April of this year for our workers’ comp patients.22
For all of its benefits, when it comes to medication management, telemedicine can be a double-edged sword, posing both risk and opportunity.
In response to the pandemic, federal and state regulators amended policies regarding prescription drugs, generally loosening restrictions to allow the following practices:
Ensuring that patients receive their medications without exposing them to unnecessary risk is a laudable goal, which can and should be achieved while exercising appropriate oversight, particularly for high-risk drugs.
Although we have made tremendous progress against the opioid epidemic, especially in workers’ comp, signs of a relapse in the general population is cause for concern. In 2019, deaths from drug overdose rose to nearly 71,000, which was an increase of 4.6% over 2018.10 Approximately 70% of drug overdose deaths in recent years have been from opioids, which brings the 2019 opioid death rate to almost 50,000,11 and all indications point to a situation made even worse by the pandemic.
Thus far in 2020, total drug deaths (including prescription and illicit drugs) are 13% higher than last year,12 an increase that is largely attributed to emotional and economic despair caused by the pandemic. When comparing suspected overdose data in the weeks before and after mandatory lockdowns, the national Overdose Detection Mapping Application Program reported an increase of 18%.13
Demand for antidepressants and anti-anxiety drugs has also increased due to the pressures of the pandemic, with new prescriptions for the month of March rising 9.2% and 10.2%, respectively.14 (Healthesystems has also seen an increase in prescriptions for antidepressants and anti-anxiety drugs among its patient population). Both antidepressants and anti-anxiety drugs pose high risks when combined with opioids, and a serious concern for workers’ comp is the possibility that these drugs are being prescribed to patients outside of their workers’ comp treatment. In addition, abuse of other drugs that are dangerous in combination with opioids, such as alcohol and methamphetamines, is also on the rise.15 All of which combines to make this a time for extra vigilance in monitoring the prescription activity of injured workers.
Antidepressant Rx’s ↑ 9.2%
Anti-anxiety Rx’s ↑ 10.2%

And this is where telehealth technology provides a valuable opportunity. In a short period of time, more patients have become familiar with and accepting of telehealth technology, which can be used to enhance patient engagement and medication management services. Connecting with patients virtually creates a safe and personal environment for pharmacists to monitor and counsel patients who may be at risk for adverse drug reactions and other complications. This type of personal connection can also help patients to feel they have a trusted healthcare resource with whom they can share any psychosocial stressors or obstacles they may experience with their current treatment regimen.

Low-risk patient ↓ 33%
High-risk patients ↓ 13%
Monitoring medication adherence during this time is extremely important, keeping in mind that standard methods of measurement may need to be re-evaluated because both medication possession ration (MPR) and proportion of days covered (PDC) could be skewed due to early refills. For high risk patients26, individual medication reviews by a pharmacist may be advisable.
As significant as the changes in healthcare and pharmacy have been, there are undoubtedly more to come in today’s dynamic environment. However, the fundamentals of patient care have not changed. Whatever the circumstances, case managers and claims professionals can still rely on tried and true best practices, such as being alert to risk factors and working with PBM partners to execute intervention strategies and actively engage patients to ensure their safe and appropriate care.
