

Applying learnings from COVID beyond the pandemic and looking to the future to protect the health of employees, as well as the downstream productivity and cost considerations for employers, is a smart strategy, given the science and statistics of infectious disease in today’s environment.
The World Health Organization (WHO) states that “epidemics of infectious disease are occurring more often, and spreading faster and further than ever, in many different regions of the world.”2 The global organization attributes this to a combination of environmental, biological and lifestyle factors that include increased cross-border travel, urbanization, population displacement due to humanitarian emergencies, conflicts and natural disasters, and unhealthy agricultural and food production practices, just to name a few.
What do these global trends mean for U.S. employers? As we continue to battle the fallout from COVID-19, it will be prudent to look at how we can “future-proof” the workplace, too.
While traumatic injuries such as sprains, strains and tears top the U.S. Bureau of Labor Statistics’ list of occupational injury types,3 illness directly related to exposure at work comprises approximately five percent of total occupational injury and illness incidence. It has been estimated in a separate analysis that on-the-job illness totals nearly $60 billion a year for both medical and indirect (productivity) costs.4
Prior to the COVID-19 pandemic, the definitions for occupational illness were typically quite narrow and predominantly applied to specific industries in which the risk of exposure at work significantly outweighs the risk of exposure in one’s daily life. For example, viruses transmitted in healthcare settings, such as human immunodeficiency virus (HIV) transmitted via needlestick injury, or infections arising from interactions with livestock in the farming or poultry industries.
But the legislative trends arising from COVID-19 have expanded how states are beginning to look at communicable diseases in the workplace – and where the responsibility for related medical costs resides. While the language and approach vary from state-to-state, 2021 saw a wave of proposals that would put permanent legislation into place allowing injured workers who contract a communicable disease in the workplace to file a workers’ compensation claim.
It’s a controversial trend. While some of the proposals are specific to high-risk occupations, such as healthcare workers, others take broader strokes. And even among these frontline jobs, a recent study demonstrated that infection prevention measures are working; the study found that nurses, who typically have a high rate of patient contact, were not at greater risk of contracting COVID due to their occupation versus their exposure to the general population.5
However, amid the uncertainty of the future, this point is certain: between the increasing global threat of infectious disease epidemics and the expansion of communicable disease presumptions, employers can’t afford not to implement strategies that will protect their workforce – and their organizations.
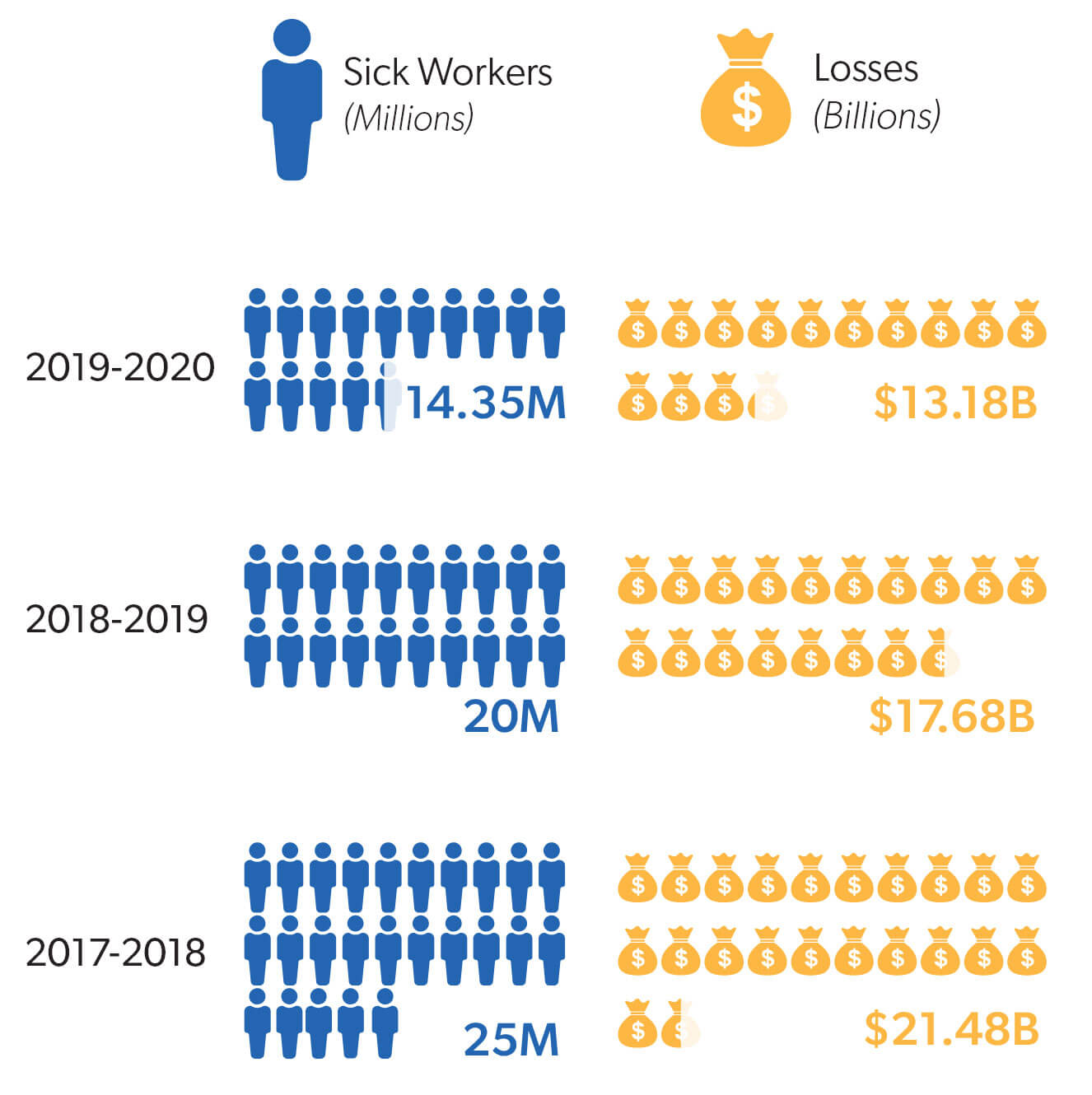
Presumptions aside, communicable diseases – even those that are not deemed occupational – cost employers significantly in terms of employee lost time and productivity. Take the common flu virus. Pre-pandemic, the 2018-2019 productivity loss estimate due to influenza was $17.6B, based on a 4-day work loss assumption per sick employee.6
To compound this, as a society, we’re getting back to the usual business of being sick. For a period, the lifestyle adjustments made during the initial pandemic peak – quarantine, work-from-home accommodations, mask-wearing – appeared to also have reduced rates of infection for other respiratory illnesses. Emergency department visits for the flu and the common cold were lower in 2020 compared with 2019.7
But as pandemic restrictions were rolled back, daycares and schools reopened, and employees returned to their worksites, these common illnesses have bounced back. In fact, according to experts at the Cleveland Clinic, doctors “are seeing more colds and respiratory illnesses this year than in the past.”8
Taking all the aforementioned factors into consideration, there are many strategies employers can employ to help reduce the risk of infectious disease exposure among their employees and create a more resilient workplace.




A key attribute of organizations that “got it right” during the pandemic? Support and communication from leadership – and this specifically means communicating with urgency, empathy and transparency, according to the Harvard Business Review.9 Regular town halls, employee bulletins, or other means of communication help employees understand current policies and expectations, as well as their individual role in mitigating risk. Regular communication can also help reduce anxiety among employees in times of crisis. Leaders should listen to employees that have concerns with return to work and accommodate when possible.
– Harvard Business Review10




1. PwC. US Remote Work Survey. January 2021. https://www.pwc.com/us/en/library/covid-19/us-remote-work-survey.html
2. World Health Organization (WHO). Managing Epidemics: Key Facts About Major Deadly Diseases. 2018.
3. Bureau of Labor Statistics, U.S. Department of Labor. Employer-Reported Workplace Injuries and Illnesses – 2019. November 2020. https://www.bls.gov/news.release/pdf/osh.pdf
4. Leigh JP. Economic burden of occupational injury and illness in the United States. Milbank Q. 2011 Dec;89(4):728-72. doi: 10.1111/j.1468-0009.2011.00648.x.
5. Jacob JT, Baker JM, Fridkin SK, et al. Risk factors associated with SARS-CoV-2 seropositivity among US health care personnel. JAMA Netw Open. 2021;4(3):e211283. doi:10.1001/jamanetworkopen.2021.1283
6. 2019-2020 Flu Season Could Cost Employers $13B. Challenger, Gray & Christmas, Inc. https://www.challengergray.com/blog/2019-2020-flu-season-could-cost-employers-13b/
7. Rodgers L, Sheppard M, Smith A, et al. Changes in seasonal respiratory illnesses in the United States during the coronavirus disease 2019 (COVID-19) pandemic. Clin Infect Dis. 2021;73:S110–S117. https://doi.org/10.1093/cid/ciab311
8. Why Does Everyone Seem to Have a Cold Right Now? Cleveland Clinic. July 2021. https://health.clevelandclinic.org/why-does-everyone-seem-to-have-a-cold-right-now/
9. Holtom B, Edmondson AC, Niu D. 5 Tips for Communicating with Employees During a Crisis. Harvard Business Review. July 2020. https://hbr.org/2020/07/5-tips-for-communicating-with-employees-during-a-crisis
10. Zak PJ. The Neuroscience of Trusts. Harvard Business Review. January-February 2017. https://hbr.org/2017/01/the-neuroscience-of-trust
