As of November 13, 2020, the World Health Organization (WHO) documented over 53 million cases of COVID-19 globally and over 1.3 million deaths,1 while within the U.S. the Centers for Disease Control and Prevention (CDC) estimated 10.8 million cases and 250,000 deaths.2
As these numbers continue to rise, COVID-19 continues to affect all facets of society and will for the foreseeable future. Narrowing the focus to workers’ comp, in Florida, COVID-19 claims made up 26% of all indemnity claims,3 while the Workers’ Compensation Insurance Rating Bureau (WCIRB) estimates that in California, COVID-19 claim costs will range anywhere from $600 million to $2 billion.4
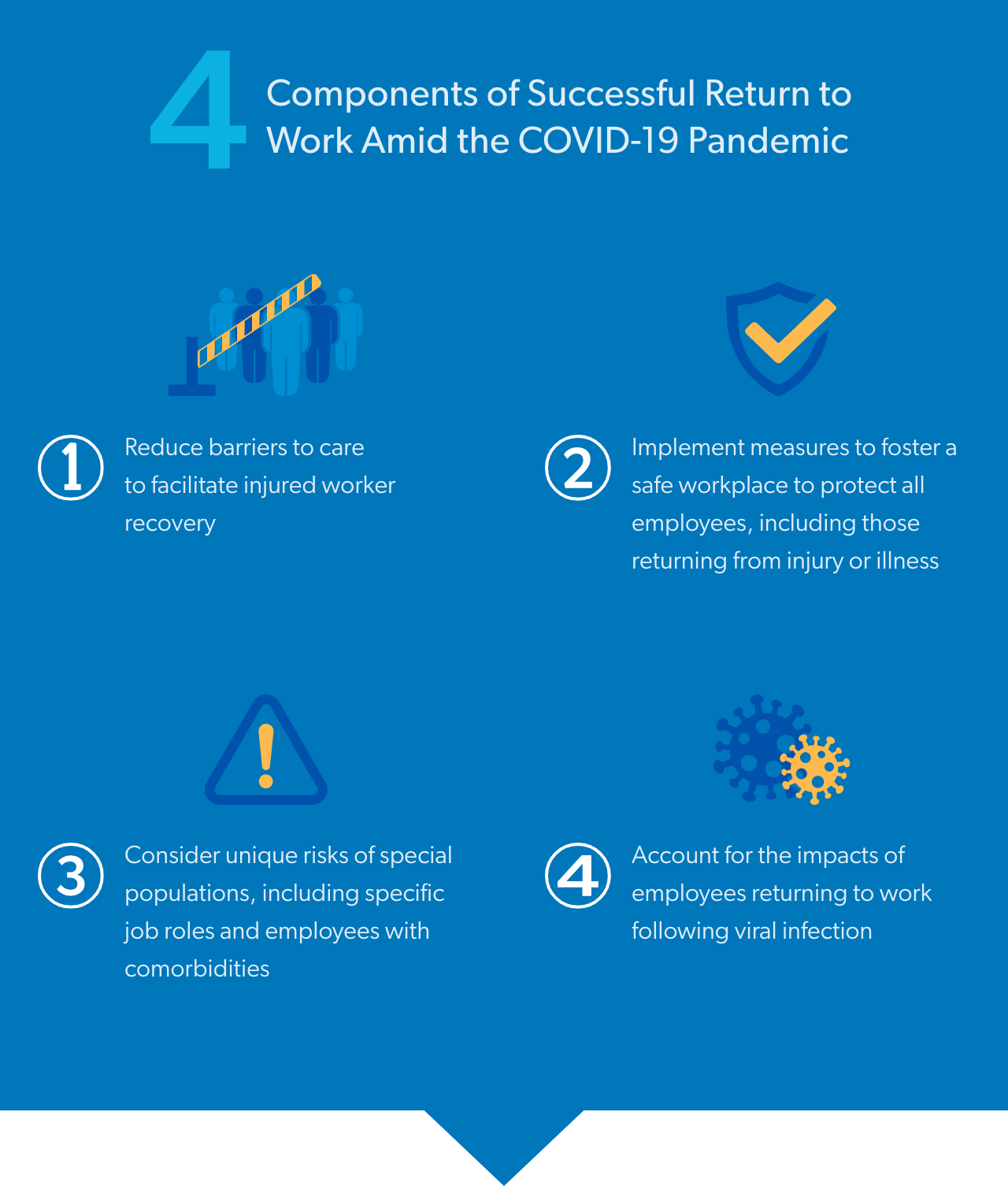
With states reopening and individuals reentering the workforce after socially isolating, the idea of what constitutes a safe workplace has changed, and the term “return to work” now takes on a whole new meaning.
In addition to the complexities of reintroducing injured workers to the workforce, employers now must incorporate risk management strategies that protect their entire employee population from viral exposure. Meanwhile, the industry is tackling other new challenges that have emerged due to the enormous and ubiquitous impact of COVID-19.
The social and healthcare protocols put in place to help manage the COVID-19 pandemic have disrupted multiple aspects of healthcare and impacted countless patients, and this may be especially detrimental to workers’ comp patients, where treatment continuity and monitoring are imperative to recovery.
A primary area of concern from the start of the pandemic has been in-person office visits, which have been relied upon in workers’ compensation to facilitate services such as physical medicine and other rehabilitative services, as well as to provide ongoing monitoring for patients receiving controlled substances such as opioids. According to the IQVIA Institutes, a multinational healthcare information technology research firm, at the beginning of the pandemic, restricted movement orders around the country resulted in a 70-80% reduction in the number of patient visits to doctors’ offices.5
From a pharmacy standpoint, concerns were originally raised that patients may face difficulty acquiring the medications needed to manage their injuries, occupational illnesses, and comorbid conditions impacting their overall health. Not only may patients not want to visit pharmacies, but potential drug shortages could impact an injured worker’s ability to access their prescribed medication.
While there is no way of knowing how further developments, such as a second wave of COVID-19, may impact refill trends or pharmacy supply, back in March, 38 million more refills were dispensed for chronic prescriptions than normal, before.5 Though this trend of stockpiling decreased after a month, further business disruptions that emerge due to impacted supply chains, drug ingredient sourcing from foreign sources, and continued economic blows, create further uncertainty.
The workers’ comp industry was quick to respond at the start of COVID-19 to address many of these barriers.
Embracing telehealth in workers’ comp programs can help patients maintain continuity of care, as various check-ups can be conducted digitally. However, these services have typically been underutilized in workers’ comp.
The Centers for Medicare and Medicaid Services (CMS) expanded access to telehealth, and dozens of state legislatures followed suit by approving emergency rules, new fee schedule rules, and other policy updates to remove restrictions that stood in the way of telehealth. In fact, the IQVIA Institutes estimate that at the beginning of the pandemic, 25% of consultations were held via telehealth.5
Workers’ comp payers can further assist patients by adjusting their programs to help simplify access to telehealth services to ensure continuity of care in areas such as telerehab, virtual translation, and other ancillary services. Telehealth services can also support ongoing monitoring and consultation that may accompany certain prescription medications.
Workers’ comp payers can also work with their pharmacy benefit management partners to ensure they are accommodating changes in Federal and State Executive Orders, emergency policy updates, and more. This includes pharmacy program adjustments that help patients obtain their medications more easily, such as relaxing parameters for mail-order, early refills, and 90-day supplies of appropriate drugs.
Clinical expertise plays an important role in addressing new and developing challenges. Clinical experts can analyze information from various medical sources to stay up to date on the latest data, identify potential medication shortages and trends that may emerge, and work to address dynamic and changing needs, with the understanding that unique patient populations have unique needs.
Furthermore, as various drugs are being used to treat COVID-19, pharmacy programs must take into account how those drugs can interact with a workplace injury, the drugs used to treat that injury, and comorbidities and their respective medications.
Drugs seen in COVID-19 claims are primarily for symptomatic control and may include:
In fact, research from the start of the pandemic found that in hospitals, medications used to treat the symptoms of COVID-19, including respiratory treatments, sedatives, and pain medications, saw increases between 100-700%.5
Once employees are ready to return to work – whether they are returning on the heels of recovery, or simply reentering their jobsite as businesses reopen – prevention of viral spread becomes a focus. There are a wide variety of safety measures that can be used in the workplace to minimize viral exposure, and the following pieces of guidance on workplace practices, communicating key information, and environmental considerations from the Occupational Safety and Health Administration (OSHA) may be of assistance.6

Encouraging telecommunications and working from home cannot be utilized for all occupations. When employees must be on-site to work, the following practices can be of assistance if they can be reasonably implemented:
Keeping employees updated and aware of best practices is always crucial, but even more so in light of this pandemic. The following tips can keep employees informed:
When possible, consider utilizing the following physical constructs and actions:
Individuals with comorbidities are at higher risk of both contracting COVID-19 and experiencing the disease more severely.
A study of 5,700 hospitalized COVID-19 patients in New York City from the Journal of the American Medical Association (JAMA) found that:7And in terms of fatalities, as of October 7, 2020, the CDC calculated that among COVID-19 deaths:8
This is particularly relevant as workers’ comp claims with a comorbid diagnosis have tripled in the last decade, and such claims typically are associated with twice the medical costs of other claims.9

The COVID-19 pandemic has increased the risk of mental distress, both from directly worrying about infection, but also from the accumulated stress of downstream considerations such as finances, employment, food, housing, childcare, a reduced support system from social isolation, and more.
This compounds the normal stress employees may have on the job, even prior to a global pandemic. The Anxiety and Depression Association of America estimates that 72% of people have daily workplace stress and anxiety that moderately interferes with their lives,10 and all of these factors are compounded by the additional stress of returning to an uncertain workplace after an injury.
Mental health issues such as anxiety, depression, and catastrophizing (assuming the worst of things), and fear avoidance can impact injured worker care. For example:
Employers can help their employees cope by taking measures to ease some of the mental burdens caused by the pandemic. This can include:
Specific to workers’ comp, the industry can do our part by ensuring programs accommodate the needs of injured workers with mental health concerns, especially in healthcare’s current state of disruption. This may include:
Occupations that are particularly vulnerable to contracting COVID-19 may cause additional downstream impacts within workers’ comp, and so it is important to understand who is being impacted the most.
Healthcare workers who care for COVID-19 patients are at highest risk, as are first responders, frontline essential workers such as grocery store employees, and more. But how do the numbers break down?
In an analysis of compensable COVID-19 claims in the Florida workers’ comp system:3
However, it is important to recognize that different states have different presumption laws and policies for covering COVID-19 infection that may have developed on the job, and so the reporting of cases could be mixed, as some claims may be ruled as compensable in one state or occupation, but not compensable in a different state or occupation.
Furthermore, as COVID-19 has created many economic shifts, there are an untold number of new developments to consider. While unemployment has gone up, the job market is changing in some areas.
For example, as consumers turn more to online shopping to avoid visiting brick-and-mortar shopping, there is a growing need for warehouse workers in distribution centers, which could become a hotspot for infection, as well as delivery drivers for outlets. There is also a growing need for delivery drivers for a multitude of businesses.
Introducing new workers into new work environments creates even more unknowns in this complex equation. As some workplace injuries commonly involve new employees, could there be minor upticks of injury frequency in certain fields? Without knowing how the economy and job market will continue to change, more of these unknown risks could be lurking, requiring a close eye on these trends.

If an employee is infected with COVID-19 and recovers, there are still several unknowns surrounding the virus, making return to work a delicate thing to consider. Overall, return-to-work evaluations should consider:14
What is known is that COVID-19 can cause acute respiratory distress syndrome (ARDS), a buildup of fluids in the lung that can reduce oxygen to the bloodstream. Approximately 50% of individuals surviving ARDS have not returned to work after one year,14 but even if they do return to work, their impacted breathing would likely require changes to workplace duties.
Currently, for patients without hospitalization, there are no quality data on returning to work, short-term disability, or long-term disability. Regarding short-term disability and return to work, recovery from post-infection fatigue is estimated to take approximately 2-3 weeks and appears to correlate with clinical duration and severity.14
In patients who have been hospitalized, general skeletal muscle deconditioning is expected in patients who are intubated for any extended duration. These patients may require exercise programs and possibly rehabilitation services.14 If such employees are later cleared to return to work, they may require lighter physical duties as their bodies continue to recover.
Many of these complex cases will need to be addressed by occupational and environmental medicine physicians.
