For over a decade, the workers’ comp industry has battled endlessly against the inappropriate utilization of opioid pain medications. The opioid epidemic has caused 400,000 overdose deaths since 1999,1 along with untold financial ramifications.
But over the last few years, the tide has been turning. Overall opioid prescribing has been declining since 2012, with a 19% reduction in the annual prescribing rate from 2006-2017.2
This trend is so prevalent that workers’ comp professionals in managed care are now shifting their attention to other matters. According to a 2020 workers’ comp industry insights survey conducted by Healthesystems, while chronic pain remains the top most concerning health risk within claimant populations, opioids are no longer viewed by industry professionals as a top program challenge, health risk, or claim risk.3
While there’s still work to be done to end the opioid epidemic, especially in regard to synthetic opioids like fentanyl, it is clear that, within the industry, different pain therapies are being embraced. Our survey data aligns with a study by the Workers’ Compensation Research Institute (WCRI) of 27 state workers’ comp systems that found prescription opioid utilization is decreasing while the utilization of other pain management therapies are on the rise.4
As the industry embraces different pain therapies, what should workers’ comp professionals know about these therapies?
Nonsteroidal anti-inflammatory drugs (NSAIDs) are widely used to treat a variety of different pains and aches for many short and long-term conditions. Commonly used NSAIDs include:
While NSAIDs are typically much safer than opioid pain medications, they do come with their own set of risks, including cardiovascular risks and gastrointestinal concerns.
NSAIDs can cause high blood pressure and increase the risk of heart attack or stroke, which can be problematic for injured workers with comorbid cardiovascular diseases, or who are taking other medications that increase blood pressure, including antidepressants or erectile dysfunction medications.
In fact, back in 2015 the FDA strengthened their warning that NSAIDs can cause heart attacks and strokes, advising patients to seek immediate medical attention if they experience symptoms of chest pain, shortness of breath, weakness in one side of the body, or slurred speech. Risk of heart attack or stroke can occur as early as the first weeks of using an NSAID, and the risk may increase with longer use of an NSAID.7
RISK OF HEART ATTACK OR STROKE CAN OCCUR AS EARLY AS THE FIRST WEEKS OF USING AN NSAID.7
Furthermore, NSAIDs can irritate the stomach and intestinal lining, leading to stomach pain, stomach ulcers, intestinal bleeding, and other gastrointestinal concerns. Patients already at risk or currently suffering from certain gastrointestinal concerns may need to avoid NSAIDs.
Acetaminophen is used to treat minor aches and pains (in addition to fever) and is much safer than opioids, while also avoiding the gastrointestinal and cardiovascular concerns associated with NSAIDs.
60 MILLION AMERICANS CONSUME ACETAMINOPHEN ON A WEEKLY BASIS8
Acetaminophen can potentially damage the liver, and long-term use can cause liver toxicity. These risks increase significantly with alcohol consumption or the use of blood thinners like warfarin. Furthermore, acetaminophen overdoses can be fatal, as they may cause liver failure.
Patients already at risk of liver disease should be cautioned against utilizing acetaminophen, as should older patients who may be more sensitive to potential liver damage.
Additionally, acetaminophen is available over-the-counter (OTC), and so a patient’s use of acetaminophen may not be documented on a claim. Furthermore, acetaminophen is contained in many combination medications, including cold medications that a patient may be taking in addition to their workers’ comp medications. Patients and claims professionals may be unaware of high-levels of acetaminophen utilization across a diverse drug regimen, which can lead to overdose.
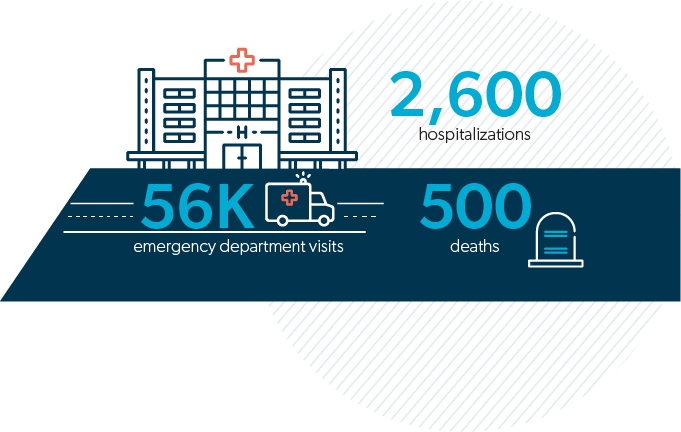
Every year, acetaminophen use results in:8
Gabapentinoids are anticonvulsant (anti-seizure) drugs used to treat neuropathic (nerve) pain. Common gabapentinoids found in workers’ comp include :
Some gabapentinoids are classified as Schedule V drugs, either federally or by select states.
Gabapentinoids contain mood-altering properties, and excessive use significantly increases the risk for suicidal thoughts and overdose. Furthermore, gabapentinoids can be abused, and they can potentially lead to serious breathing difficulties.
One study of 190,000 people found gabapentinoid users experienced:10
Law-enforcement data has found that gabapentinoid diversion is on the rise,11 as these drugs can be used in high doses to achieve a high, similar to intoxication.
Growing misuse and abuse of gabapentinoids has caused Ohio and Massachusetts to require the dispensing of gabapentinoids to be reported to prescription drug monitoring programs (PDMPs). Ohio alone saw 426 million solid oral doses dispensed to patients in 2017.14
Furthermore, the FDA issued a warning that serious breathing difficulties may occur in patients using gabapentinoids who have respiratory risk factors, including respiratory disease like chronic obstructive pulmonary disease (COPD). These risks are further amplified among older populations.15
Muscle relaxants are used to alleviate muscle spasms and pain in workers’ comp. Several muscle relaxants are classified as Schedule IV drugs. Common muscle relaxants in workers’ comp include:
Muscle relaxants should only be used short term, as adverse effects include mood change, impaired thinking, paralysis, central nervous system (CNS) depression, respiratory depression, and heart failure. Patients already at risk for these factors may not be ideal candidates for muscle relaxants, and overuse of muscle relaxants can lead to dependence, withdrawal and abuse.
The U.S. Poison Centers found that one muscle relaxant alone, baclofen, saw toxic exposures increase by 36% from 2014-2017, with admission to a healthcare facility required in over half of those cases.12 Meanwhile, emergency department visits doubled between 2004 and 2009 for carisoprodol, another common muscle relaxant.16
Physical medicine focuses on restoring functional ability to patients facing physical impairments, which may result from workplace injury, primarily through active physical exercises or manual therapeutic techniques.
Physical medicine services in workers’ comp may include physical therapy, occupational therapy, and work hardening and work conditioning. The Centers for Disease Control and Prevention (CDC) recommend the utilization of physical therapy for treating chronic pain,17 and medical research has established that physical medicine can:
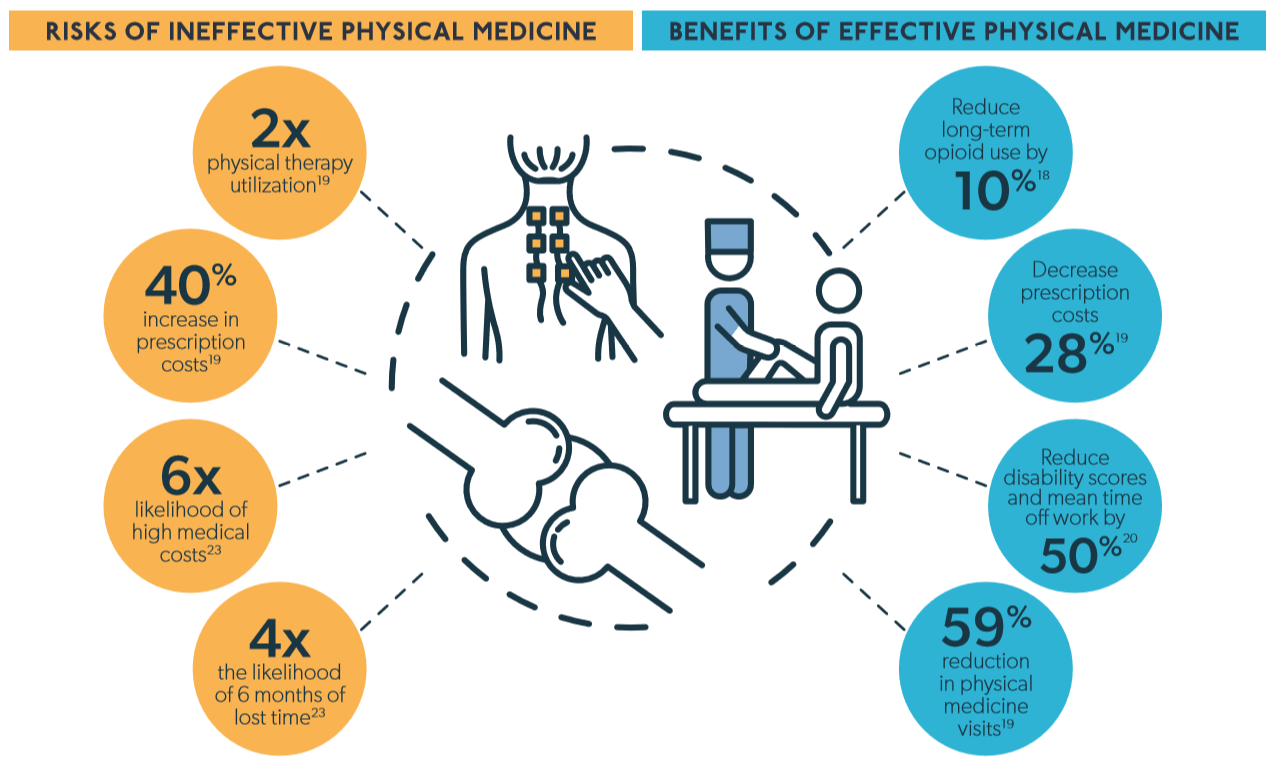
While physical medicine can do well for treating the root cause of pain, this is only the case when physical medicine is effectively managed.
Non-adherence to physical medicine evidence-based guidelines can double treatment utilization, while increasing prescription costs by up to 40%.19 Meanwhile, evidence-based physical medicine can reduce the number of physical medicine visits by 59%.18 This indicates that using appropriate modalities is critical to controlling overall utilization.
Furthermore, claims with 15 or more physical therapy visits were six times more likely to result in high medical costs and four times more likely to result in six months of lost time.23 While the need for so much physical therapy could be tied to the severity of injury, hence a need for more frequent care, it is also possible that so many visits could signal ineffective utilization.
Effective physical medicine requires transparency into the services delivered, along with their costs, and the clinical metrics taken from each visit, which can be used over time to measure the effectiveness and value of service.
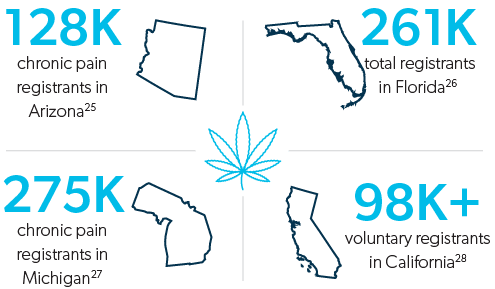
Over the last decade, medical marijuana has seen an increase in support from the general public, academic researchers, and clinicians across the country. Though there is much confusion and controversy surrounding the use of marijuana for pain, as it is a Schedule I controlled substance, there is clinical evidence that marijuana can benefit patients experiencing chronic pain and neuropathic pain.24
In fact, one systematic review and meta-analysis of 79 trials found that marijuana use, when compared to placebo, yielded:24
Growing support for marijuana has led to many prescribers recommending the drug for the treatment of pain. In fact, legislators in New York, Illinois, and Colorado allow patients to swap out opioid prescriptions for medical marijuana.
First and foremost, marijuana should not be a first-line treatment for chronic or acute pain, and should only be reserved for use when other, more traditional therapies fail. There is also still a significant lack in clinical research as to the long-term impacts of marijuana therapy, which creates confusion surrounding:
And of course, marijuana comes with its own set of inherent risks.
In the last several years, there has been a growing interest in alternative medicine, including modalities for the treatment of pain. While there is a wide variety of alternative therapies available, clinical research has found that the following modalities could help reduce chronic pain:29-33
With so many different alternative therapies available, it may be difficult to keep track of the growing research surrounding each therapy. However, it is important to differentiate alternative therapies that may offer clinical benefit from those that do not.
Whether or not it is visible on a claim, injured workers could be utilizing alternative therapies in addition to, or in replacement of, their managed care treatment. When an injured worker takes additional medications for a comorbidity not related to injury, that medication may not be visible on a claim, potentially leading to drug-drug interactions. In the case of supplements, herbal remedies and other ingested materials, this is no different.
Furthermore, it is important to understand the qualifications the various providers of these services possess. Inappropriate practices could jeopardize patient health and discerning the validity of certain practitioners could be difficult.
As prescribers continue to shift away from opioids and towards other therapies for pain, claims will continue to grow more complex. We may know what happens when faced with high opioid utilization, and we may already have program strategies to counteract these effects, but these prescribing shifts foreshadow new developments in store for claims management.
While moving away from opioids is likely to reduce overall risk, new risks may lie in store, requiring a growing awareness of new and evolving factors. Partnering with a strong PBM partner can provide clinical guidance on a multitude of therapies and help insurers to facilitate and address further industry developments in the treatment of pain.
Just as the use of opioid medications requires various considerations, so does the use of other pain therapies.
When utilizing non-opioid pain therapies, it is important to consider factors such as age, gender, ethnicity, comorbidities, and other personal health matters, as these attributes can greatly impact the safety and effectiveness of therapy.

One alternative therapy that has seen growing popularity lately is acupuncture, the practice of inserting needles into the body to relieve pain.
Previously dismissed by western medicine, not only have systematic reviews of medical literature demonstrated that acupuncture could be useful in reducing chronic pain,29 but certain clinical trials found that acupuncture could be more effective in improving symptoms of low-back pain than NSAIDs,38 and that claims involving acupuncture more consistently saw lower-dose opioid use.17
While more research is necessary to definitively establish acupuncture’s effectiveness in the treatment of pain, New York, California, and Washington State cover acupuncture in workers’ comp to varying degrees, as does the Center for Medicare and Medicaid Services.
