Managing the complexities of claims is more important than ever – but as we continue to peel back the layers of what drives the duration, cost, and patient safety concerns associated with complex claims,1 in some ways it is becoming more challenging than ever. And as we as an industry continually develop new and innovative tools to help address these challenges, there is one asset that can perhaps be leveraged more optimally as a mitigator of claim complexity – the injured worker patient.
Even as workers’ compensation programs have been moving towards a more patient-centric approach to managed care, injured worker patients themselves may not always be positioned as equal stakeholders. To some extent, they move through the claims process as the object in Newton’s third law of motion, upon which the forces of the system, however well-designed or intentioned, are applied.

This may lend some insight into why aspects of the claims process may involve the injured worker in a unidirectional fashion, delivering information without a structure or process in place that invites patient input.
But what if more aspects of the claims process were built to better accommodate the flow of information in both directions? Consider one example where the injured worker is involved in their claims journey from a bidirectional standpoint in their own claims experience – the initial reporting of an injury.
This is just one example; there are opportunities throughout the claims process where patient education and engagement, and especially engagement that invites a bidirectional flow of information, can work to mitigate these complexities. These opportunities can be powered by human interaction, through technology, or ideally, both – whether it is tools and processes that allow injured workers to self-report on progress throughout their recovery, or high-touch, clinically driven interventions that invite direct dialogue.

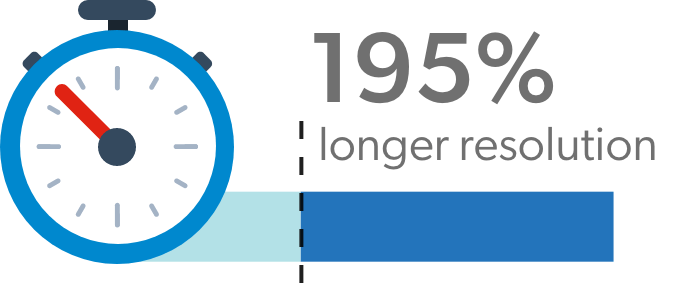
Consider, also, the other end of the spectrum. Litigation was among the top 5 factors contributing to claim complexity as reported by workers’ comp professionals in Healthesystems’ study.2 And it is a powerful example of how a breakdown in the relationships between the injured worker and other stakeholders can have a significant negative impact on the outcomes of claims.
A breakdown in communication can be a driver of litigation in the first place.2 And like a negative cycle, litigation can further shut down potential opportunities for the injured worker patient to directly engage in the workers’ compensation process. Advice on attorney websites may even include recommendations for injured workers to hide important context that can help guide more informed claims management, such as mental health or socioeconomic impacts the worker may be experiencing.