The health effects of alcohol have been well-researched for decades, but they have done little to slow down excessive drinking, with an estimated 1 in 6 Americans regularly engaging in binge drinking,1 and approximately 14.5 million suffering from alcohol use disorder (AUD), representing nearly 6% of the U.S. population 18 years of age or older.2 Unfortunately, this is no surprise, considering how omnipresent alcohol has been in human history.
The earliest evidence of alcohol can be traced to 7,000 BC China in ancient rice wine.3 The Egyptians brewed beer as early as 3,400 BC,4 and alcoholic distillation is theorized to have begun in 3,000 BC in India.5 Virtually every culture has developed some unique alcoholic beverage, often rich with history and pride.
Drinking culture is unlikely to disappear anytime soon, and while alcohol can be enjoyed responsibly, far too often it is not. The sheer pervasiveness of alcohol in the world can often blind people to the real-world impacts it can have, and workers’ comp is no exception to these impacts.
Alcohol can increase the likelihood of workplace injury and create problems in the workplace. It can also cause a wide range of health consequences that can impact claims management and injured worker recovery, and it can interfere with various medications prescribed in workers’ comp, further complicating recovery.
Industries with the highest rates of heavy alcohol use include mining, construction, and food service7
Alcohol use disorder contributes to over 232 million missed workdays annually8
Workers with alcohol problems are 2.7x more likely to have injury-related absences9
Excessive alcohol use is responsible for a $179 billion loss in workplace productivity10
Excessive alcohol use is responsible for $28 billion in healthcare spending10
Problematic alcohol use is by no means a new problem, but the COVID-19 pandemic increased the U.S. population’s use of alcohol as a response to severe stress, isolation, and uncertainty.
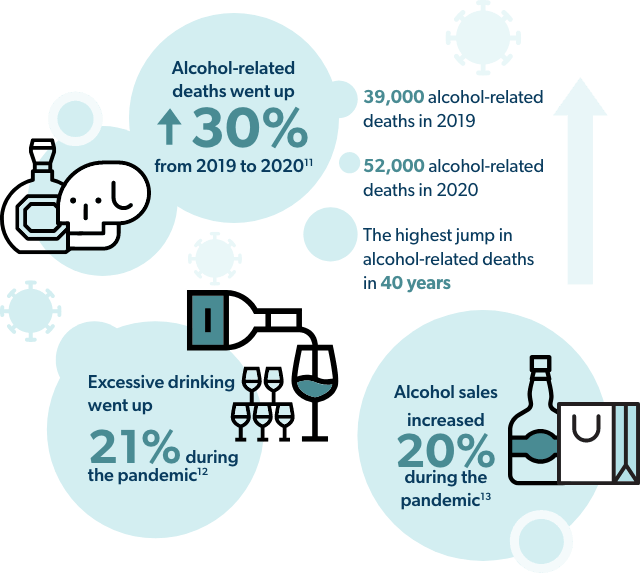
Now more than ever, it is incredibly important to understand the impact alcohol has on the work environment, the health considerations across workers’ comp claims, and how alcohol can interfere with pharmacy management.
Employees with problematic alcohol use can cause several different types of issues within the workplace, including issues of workplace safety, liability, and performance and productivity losses.
When it comes to understanding what amount of alcohol use is problematic, there are two different forms of over-consumption.

First and foremost, working while under the influence of alcohol is problematic, as drops in coordination and reaction time lead to a greater likelihood of accidents and workplace injury.
However, even when employees with problematic drinking are not inebriated on the job, there are still potential safety risks tied to hangovers. Hangovers negatively affect cognitive function, working memory, and psychomotor speed.16 This can still be the case when individuals no longer have alcohol in their system but are still experiencing a hangover.
Problematic alcohol use among employee populations can create financial strain for employers, stemming from missed workdays, drops in productivity and greater healthcare costs.
When consumed, alcohol travels down the esophagus and into the stomach. At this point, some alcohol passes into the bloodstream via the lining of the stomach and then travels throughout the body, impacting the brain, kidneys, lung, and liver. Meanwhile another portion travels through the small intestine.
Along this journey, alcohol has the potential to disrupt a wide range of bodily functions. The list of health risks that come with excessive alcohol use is significant, and many of these risks can add an additional layer of complexity to workers’ comp claims.
However, it is important to recognize that problematic alcohol use can be divided into two specific forms: binge drinking and heavy drinking.
While binge drinking and heavy drinking share many risks, the nature of these drinking habits can manifest quite differently. Functional alcoholics who are heavy drinkers may not drink as vigorously as binge drinkers and may be more prone to long-term health conditions and alcohol use disorder, while binge drinkers may be more susceptible to the more immediate health risks from the sheer level of alcohol they consume in a single instance.
Considering the journey that alcohol makes throughout the body, excessive use over a chronic period of time creates a wide range of health risks, all of which can make managing a workers’ comp claim far more complex.
Alcohol can negatively interact with several medications, impacting how the body absorbs, metabolizes, distributes, and excretes them. This can exacerbate certain drug effects or lead to harmful interactions, increasing the likelihood of adverse events.
Some of the potential drug interactions that alcohol can have with medications prescribed in workers’ comp include but are not limited to:
Mixing NSAIDs with alcohol can increase the risk of stomach bleeding and ulcers
NSAIDs make up 18% of Rx drug payments in workers’ comp18
Mixing alcohol with opioids can cause excessive drowsiness, respiratory depression, and death
1 in 7 opioid-related deaths involved drinking alcohol within a few hours of opioid use19
Both gabapentinoids and alcohol cause CNS depression and respiratory depression, creating risk for therapeutic duplication. Additionally, mixing alcohol with gabapentinoids can increase risk of seizures
Gabapentinoids are among the top three drug classes prescribed in workers’ comp20
If the liver is breaking down alcohol, it cannot break down acetaminophen. This can lead to a buildup of acetaminophen, which can cause liver damage
Increased sedation, muscle fatigue, trouble balancing, intense confusion and paranoia, disinhibited actions, respiratory depression which can be fatal, suicidal thoughts
Alcohol was involved in 21% of benzodiazepine drug-related deaths21
Depression and anxiety, confusion, dizziness and trouble balancing, impaired judgment, motor skill impairment, poor memory and difficulty concentrating, respiratory depression, overdose, and death
This drug interaction can cause dizziness, fainting, drowsiness, and a faster heartbeat
Alcohol can exacerbate the sedative effect of anti-anxiety medications, causing drowsiness or unconsciousness
Mixing alcohol with antidepressants can affect judgment, coordination, motor skills, and reaction time. This can also cause drowsiness and confusion
Combining alcohol with diabetes medications can lower blood sugar, create rapid changes in blood pressure, and increase heartbeat
Whether through wellness programs, employee assistance programs (EAPs), or benefits available through group insurance, there are treatments for problematic alcohol use that are effective when properly utilized.
However, the initial step is identifying patients who need help and connecting them with resources that can help them. 14.5 million Americans have alcohol use disorder (AUD), but less than 10% of them receive treatment.2
Within the scope of workers’ comp, the larger conversation of gaining visibility into social and behavioral determinants of health has gained serious traction. With social and behavioral factors comprising upwards of 80% of modifiable factors impacting health outcomes,23 it stands to reason this is such a strong area of focus. Traditionally, identifying claims where one or more social or behavioral determinants are a negative contributing factor could be compared to finding a needle in a haystack – especially a factor such as AUD, which affects less than 6% of the U.S. adult population. But identifying these factors needn’t be so difficult. We have the clinical tools and technology to get us there today at lightning speed.
Take physical therapist (PT) notes as an example. As a provider who spends significant, quality time with the injured worker, a PT is well positioned to gain insight about the injured worker that can help identify social and behavioral barriers to recovery (see A Golden Opportunity: The Physical Therapist’s Role in Behavioral Health in this issue of RxInformer ). And this needn’t be a heavy lift for provider or patient. A study utilizing a questionnaire used by the Institute of Medicine designed to capture social and behavioral determinants of health took an average of 5 minutes for patients to complete and garnered an 80% participation rate in the first week of the study.24
By Healthesystems’ estimation, each PT episode of care generates, on average, more than 50 pages of PT notes. And these documents are rich with insights – including those of a social and behavioral nature. Here is where technology comes into play – helping to analyze data at scale, taking those individual, 1-on-1 PT interactions and aggregating them across a claims population. An analysis of evaluation and functional capacity forms from approximately 100,000 episodes of care conducted with natural language processing (NLP) technology revealed a SDoH documented in approximately 80% of claims.25
Keep in mind that this is just the tip of the iceberg. PT documents represent just one of many documented data sources present on a claim. And within this, evaluation and functional capacity forms represent just a fraction of PT documents.
So what did this targeted analysis reveal about AUD? Substance abuse, including alcohol abuse, was in 1 of 50, or 2.5% of claims. Perhaps most impactful is the timing aspect, with approximately 1 in 3 of these claims being identified within the first 30 days of injury through data captured at the initial evaluation, and 85% identified within 90 days of injury. Early identification provides earlier opportunity to intervene, a significant advantage in helping to address the downstream clinical complexity of a behavioral risk such as AUD, which is associated with extended treatment durations as well as a higher frequency of missed PT appointments.
Behavioral treatments that aim to change drinking habits through counseling have proven to be effective. Among many forms of therapy, this includes cognitive behavioral therapy, which helps identify feelings and situations that lead to heavy drinking, with the goal of changing these thought processes to develop skills necessary to cope with everyday situations that trigger drinking.23
In addition to therapy, there are three FDA-approved medications that can help stop or reduce drinking and prevent alcoholic relapse. They include:26
One key point to note is that if an injured worker is receiving medication-assisted therapy for alcohol abuse, there are potential pharmacy management issues that can arise from mixing any of these medications with other medications used to treat a work-related injury or illness.
If you or anyone you know is struggling with alcohol abuse, SAMHSA’s National Helpline, 1-800-662-HELP (4357) is a free, confidential, 24/7, 365-day-a-year treatment referral and information service (in English and Spanish) for individuals and families facing mental and/or substance use disorders.26