Pharmaceutical research & development has become laser-focused on the development of specialized drugs, producing some very significant drug innovations over the last several years. The crop of new hepatitis C (HCV) antivirals that first hit the market in 2015 presented hope for converting a chronic disease into one that is instead curable. The same year brought the approval of the United States’ first biosimilar product, which opened the door to greater access and affordability of biologic medications. And this August, the FDA approved the first gene therapy in the U.S., a treatment for select patients with acute lymphoblastic leukemia (ALL), a form of cancer for which few treatment options exist.
Drug innovations such as these provide the opportunity to bridge existing gaps in care and reduce the morbidity and mortality associated with chronic and life-threatening conditions. But what role do they currently serve in the care of workers’ compensation populations?
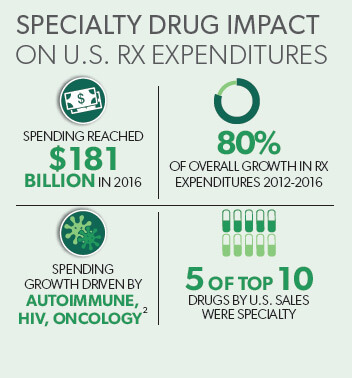
In short: a growing one. Specialty medications have been making their way into workers’ comp claims over the last several years akin to the way a stream is formed. Beginning with a small trickle, and over time carving out a path that gradually becomes both broader and deeper. Broader, as clearer links between certain occupations and illness are established. Deeper, as the cost associated with these medications continues to set new pricing milestones.
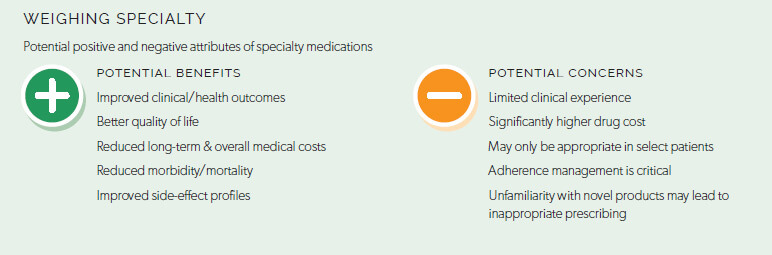
Many workers’ comp payers have seen their proportion of specialty drug spend among total pharmacy costs increase by less than 1% over the last year.1 But individual claims impacted by these medications can become dramatically more expensive when considering these therapies can cost up to 40 times more than traditional medications. Specialty spend across healthcare continues to grow, and continued growth is expected among workers’ compensation claims as well.
Because specialty conditions represent a small minority of workers’ compensation populations (less than 10 percent), drug formularies traditionally do not include specialty medications. Formulary management can be a useful tool in controlling drug selection and broader use of specialty drugs where traditional drugs may instead be appropriate, as well as controlling associated pharmacy costs. However, it can also present barriers to access for patients with legitimate medical need.
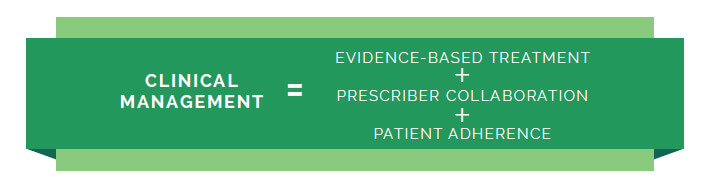
While drug prices are a prevailing conversation around specialty medications, it’s important to also consider critical care decision points that impact disease and overall cost management. For example:
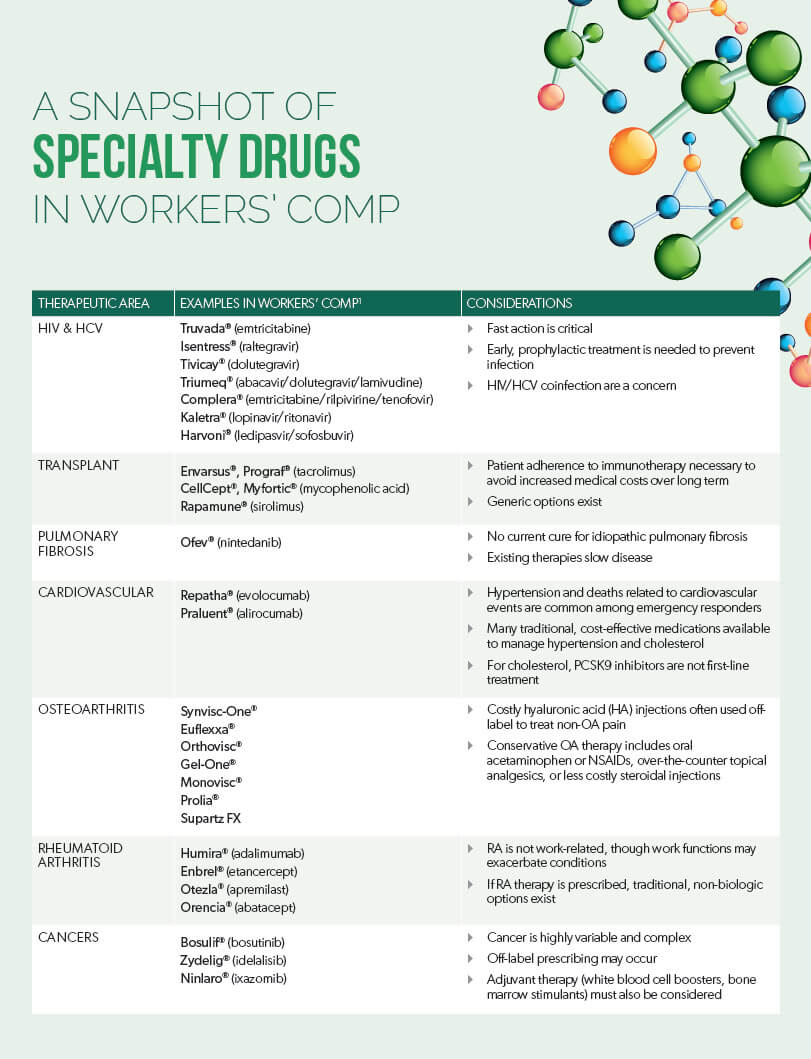
Following are 6 specialty conditions impacting workers’ compensation claims, and important considerations for managing these populations.
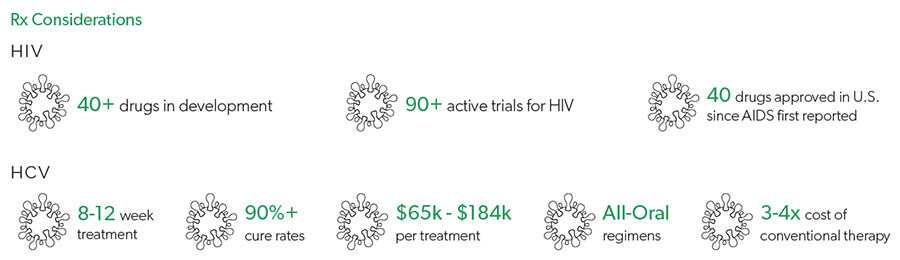
Needlestick and sharps injuries in the workplace can expose healthcare workers such as nurses or emergency department workers to infectious diseases, the most common being human immunodeficiency virus (HIV), hepatitis C, and hepatitis B.3 The Centers for Disease Control and Prevention (CDC) estimate that approximately 385,000 sharps injuries occur among hospital workers each year.4
For workers exposed to HIV and/or HCV, time is of the essence. When a worker comes into contact with HIV-infected bodily fluids, prophylactic treatment should be initiated immediately; typically, both HIV and HCV prophylactic treatment are initiated due to risk for coinfection. Delaying treatment can increase the risk for infection, translating into chronic and potentially life-threatening illness that will require ongoing treatment for the duration of the patient’s lifetime.
There are important considerations when managing treatment of acute HCV infection. While newer agents come at considerable expense, higher cure rates decrease the likelihood that the patient will progress to chronic HCV. Newer therapies also offer the benefit of not requiring co-treatment with interferon, a drug with severe side effects traditionally used to treat certain viral infections and cancers. However, newer therapies also have increased risk for certain drug-drug interactions, and insight into a patient’s overall drug regimen is critical.

Injured workers undergoing transplant due to organ injury will require long-term treatment with immunosuppressive agents, and adherence is essential.
While generic immunosuppressant options exist, specialty brands can cost upwards of $5,000 per script.1 Additionally, nonadherence to immunosuppressive therapy can cause the body to reject the transplanted organ, leading to a potential need for re-transplantation, an increase in healthcare costs, with a higher risk of death. Thus, there are benefits to dispensing these medications through a specialty pharmacy program that incorporates clinical management focused on improved adherence, patient education, and counseling services.

Pulmonary fibrosis is a disease in which deep lung tissue becomes scarred and thickened, impeding the ability to breathe. Occupational/environmental pulmonary fibrosis can occur in occupations including miners, millers, foundry and quarry workers, and sandblasters due to exposure to airborne particles such as asbestos or silica. However, there is also evidence of certain occupational/environmental risk factors for idiopathic pulmonary fibrosis (IPF), an irreversible and fatal form of the disease.5-7
Treatment of pulmonary fibrosis is dependent on the severity of disease, which is highly variable. For severe and progressive cases, it is important to realize there currently is no cure, and that even the newer therapies can only slow the disease.

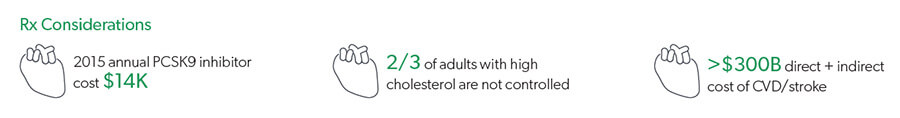
Emergency responders are at higher risk for cardiovascular (CV) conditions such as hypertension and high cholesterol because of factors that include disruptions to the metabolic syndrome due to shift work and abnormal sleep patterns, noise exposure, occupational stress, and irregular physical exertion.8 Approximately 3 of 4 emergency responders are hypertensive or pre-hypertensive, and cardiovascular disease events account for 45% and 22% of on-duty deaths among firefighters and police, respectively.
There is a heavy nonpharmacological aspect to the management of CV conditions in emergency responders. However, pharmacological management must also be considered. There are many traditional, cost-effective medications available to manage hypertension and cholesterol. Specialty PCSK9 inhibitors are not a first-line treatment for cholesterol management. It is also important to consider whether the side effects of any medications prescribed to emergency responders could present occupational safety concerns (e.g., dizziness, somnolence).
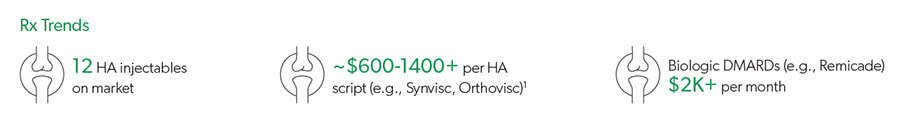
The prescribing of medications for certain inflammatory conditions in workers’ compensation often enters a gray area. Osteoarthritis (OA) is a common form of arthritis that can be caused by multiple factors, which may include occupations such as mining, construction, agriculture, and sectors of the service industry, due to the physical demands of these jobs.9,10 Rheumatoid arthritis (RA), however, is an autoimmune disease that is not considered to be directly work-related. Yet both OA and RA medications are prescribed under workers’ compensation claims.
Specialty drug trends for OA include viscosupplementation, which is the injection of hyaluronic acid (HA) products for treatment of OA in the knee. Market share of these products continues to increase, with the most recent addition of Durolane®, an HA injection approved in September 2017. Specialty RA trends center around biologic disease-modifying antirheumatic drugs (DMARDs) to suppress the body’s immune system. A common example is Humira® (adalimumab), which is currently the #1 therapy in the United States based on spend.
It is important to understand that these therapies, especially OA medications, may be prescribed off-label in workers’ compensation, and not necessarily in the context of OA – a determination that may be extremely difficult when diagnosis is unclear or inaccessible to the workers’ compensation claims professional.
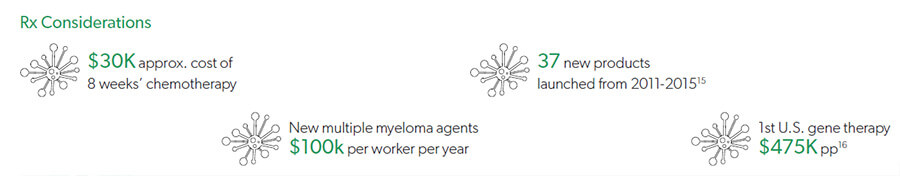
Occupational cancers can occur due to exposure to cancer-causing agents in the workplace environment, and it is estimated that 4% of all U.S. cancer cases are caused by occupational exposure.11 The CDC estimates that approximately 46,000 – 92,000 new U.S. cancer cases in 2012 were attributable to occupational exposure.12 Examples of work-related cancers are lung cancer and mesothelioma related to
asbestos exposure, multiple myeloma, which can occur in workers exposed to radiation or petroleum, and non-Hodgkin lymphoma,
which has been linked to pesticides in the agricultural industry.13,14
Cancer is a variable and complex area of medicine for which there is no one-size-fits-all approach. Determining work-related causality is often not black-and-white due to factors such as complexity of disease, disease latency, and individual patient factors. Treatment and duration of therapy are equally as complex based on appropriate agent selection and the variable types and stages of cancer. Because of these complexities, treatment guidelines allow oncologists to tailor treatment appropriately for individual patient circumstances, and off-label prescribing can be a common practice in this therapeutic area. In addition to the primacy cancer therapies, adjuvant therapy and its cost must also be considered, as patients will also receive treatments that could include white blood cell boosters and bone marrow stimulants to help offset the adverse effects of chemotherapeutic agents.
Since the introduction of morphine for the medical treatment of pain a century ago, there has been a dearth in drug innovation related to pain management. Fast-forward a couple of years, and pain medications may very well be at the top of this specialty trends list.
With opioids falling out of favor, researchers are exploring alternative, non-opioid pathways to address pain. Most notably, in August 2017, the U.S. Food and Drug Administration (FDA) fast-tracked tanezumab, an investigational, non-opioid biologic for the treatment of osteoarthritis and chronic low back pain. And there is a rich pipeline of other non-opioid products in development (see New Pathways in Pain Management: Novel Non-Opioid Medications).
While non-opioid alternatives could fill an important gap in chronic pain management, the introduction of specialty medications in this area of healthcare would have an enormous financial impact for workers’ compensation carriers, especially if these new treatments become adopted into evidence-based guidelines.