Visibility into psychosocial and mental health factors – and the influence they have on work-related injury and recovery – continues to be a key area of focus for workers’ compensation stakeholders. More than a third of respondents to the Workers’ Compensation Industry Insights Survey, conducted by Healthesystems in partnership with Risk & Insurance®, identified psychosocial factors as a barrier to injured worker recovery. And respondents as a whole ranked psychosocial factors and/or social determinants of health as the #3 component of workers’ comp claims management into which they want more visibility.1
While a significant component of psychosocial factors includes psychological factors such as anxiety, fear avoidance, catastrophizing, or depression, perhaps even more nuanced are the social components – the factors that aren’t defined in the DSM-5, that don’t have an ICD-10 code, and which can’t be addressed through medical treatment.
In our Social Determinants of Health Article Series, Healthesystems will spotlight several SDoH that impact injury and recovery, with a goal of answering these questions:
What are social determinants of health (SDoH)?
How do SDoH intersect with management of the injured worker?
What are some specific examples of how SDoH can impact workplace injury and its recovery?
How can workers’ compensation stakeholders gain more visibility into SDoH among injured worker populations?
Social determinants of health, as defined by government organizations including the Centers for Disease Control and Prevention2 and the U.S. Office of Disease Prevention and Health Promotion,3 are the conditions in the places where people live, learn, work, and play that affect a wide range of health and quality-of-life risks and outcomes. More broadly, this is inclusive of factors such as access to quality healthcare and education, economic stability, social and community dynamics, and an individual’s environment.
While we have long been aware of SDoH, there has been a continued increasing focus on them, and specifically efforts toward incorporating strategies that measure and address them in the broader healthcare ecosystem. In early 2021, the Centers for Medicare & Medicaid Services (CMS) issued guidance to states on adopting strategies that address social determinants of health in the Medicaid and Children’s Health Insurance Program (CHIP).4 In February of 2022, CMS also began soliciting feedback on SDoH-related measurement concepts to include the development of a Health Equity Index as an enhancement to the Part C and D Star Ratings program, as well as a measure to determine how well plans are screening members for health-related social needs like food, housing and transportation needs.5
5 Core Areas of Social Determinants of Health2
The impact of these issues on overall health outcomes has been well documented. It is often cited that medical care accounts for only approximately 10-20 percent of the modifiable contributors to healthy outcomes, and SDoH comprise the other 80 to 90 percent.6
This can feel like a defeating statistic, given the resources and effort put into developing medical management strategies intended to ensure injured workers are getting appropriate, cost-effective care that will position them for a successful recovery. It’s a reminder that when it comes to patient care, there are rarely any guarantees or straight paths. Individuals are complex, and while the scope of workers’ compensation is focused on managing the work-related injury, that injury is part of a person, and that person brings inherent and unique complexity that can’t be separated out.
Injured worker behavior and/or nonadherence to treatment are viewed as the #1 barrier to recovery – and behavior is in large part driven by social and environmental constructs.

Indeed, injured worker behavior and/or nonadherence to treatment was identified as the #1 barrier to recovery in the industry survey1 – and behavior is in large part driven by social and environmental constructs.
And while any SDoH has the potential to influence workers’ compensation outcomes in the same way they influence broader health outcomes, some may be especially impactful to injured worker recovery and/or services utilized in the course of their care. Does the worker have the emotional support they need at home to stay engaged and motivated in their care and recovery? Do they have the transportation they need to attend a scheduled medical appointment? Is there a substance use disorder present that a provider should consider when making prescribing decisions, especially regarding opioids or other controlled medications that pose risk for dependence, addiction or misuse? Or, do the conditions at their workplace present a higher risk that they will be injured in the first place, or potentially reinjured upon return to the workplace?
As stakeholders in the management of injured workers, what can we do to address these barriers? To begin, we can be aware of the context. We can find ways to identify when social barriers exist, and understand how they may subsequently present barriers to recovery, so that we can partner together to overcome them.
There are ripe opportunities for workers’ compensation stakeholders to gain the visibility they seek into SDoH, and those opportunities are best formed by partnering personal interaction with technology. First – are the right, quality interactions happening between injured worker patients and the appropriate stakeholders? And secondly, how are we gaining insight from those interactions? Are the right communication channels in place? And how can we best use next-generation technologies, such as AI-driven analytics and natural language processing (NLP), to consolidate and glean insight from the often disparate and unstructured data that results from these interactions?
The injured worker intersects with a multitude of stakeholders throughout their journey through the workers’ compensation system. Every interaction is an opportunity to gain insight into barriers to recovery, but some stakeholders are better positioned than others to observe potential SDoH-related barriers specifically. Home health aides, for example, have direct insight into a patient’s home life and social environment. A physical therapist who spends significant portions of 1-on-1, in-person time with the injured worker is a stakeholder who often will uncover or observe SDoH influence.
Opening lines of communication with these types of providers can help bring these insights to the claims adjuster. Right now, this is an area of opportunity for the industry, with 64% of claims professionals reporting difficult in obtaining information from medical providers.1 And in the instances where this is already happening at an individual level, how can this information be scaled for a claims adjuster across the multitude of notes and data sources associated with a claim? Enter the role of technology.
Because social barriers are tightly woven into a patient’s everyday life and overall well-being, they can present themselves in a number of (not always obvious) ways and through a number of data sources.
The key to successfully applying technology to identify social determinants of health influencing claims populations is by including as many viable, quality sources for data-mining as possible– in other words, are we broadening our data sources enough to include the volume of information required to produce accurate insights with a high confidence level across a population?
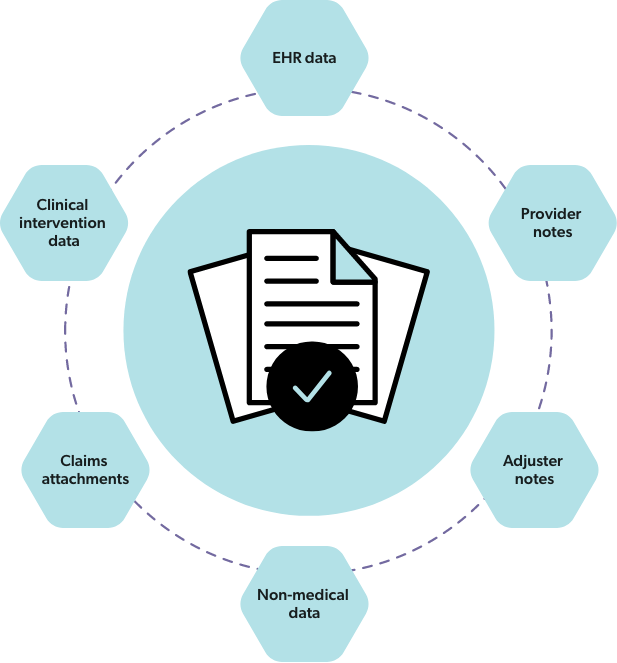
Viable sources often include the medical record, a rich amalgamation of EHR notes, physical therapy notes, adjuster notes, and any other attachments to a claim. This information can be supplemented with data gathered from clinical pharmacists through direct interventions with injured worker patients and other key stakeholders involved in their care. And non-medical data can also prove to be valuable sources, such as data gathered from investigative services. Going beyond a single set of documents, such as physician notes, to include information captured by other providers or sources, can help fill in any gaps.
Once the viable data sources have been identified, NLP allows a machine to process and analyze large amounts of natural language text and extract the key data elements that provide insight and context to SDoH-driven claim complexities. Rather than applying valuable human resources to read through individual medical records or other documentation, data extracted through NLP can quickly point to the most pertinent information within each claim.
When applied to all viable records across a patient population, all of this unstructured data can be stored as discrete data elements to inform increasingly refined analytical models. Other artificial intelligence and machine learning tools can process large amounts of data, auto-segmenting the claimant population and assigning risk and severity scores. The more data there is to work with, the more accurate these models become. So, as NLP combs through each patient record for information to inform individual patient risk, it also provides data that will help predict larger population performance as it relates to social barriers.
